![]()
Age-related macular degeneration (ARMD) affects 10 million Americans each year. The number of cases is expected to rise as we are living longer.
- How do you prevent getting macular degeneration?
- If you have a family history of age-related macular degeneration, does that mean you will get it?
- Is there anything you can do to improve my sight if I currently have ARMD?
More research and funding are being dedicated to this disease than ever before, yet there is still much we do not know.
What is macular degeneration?
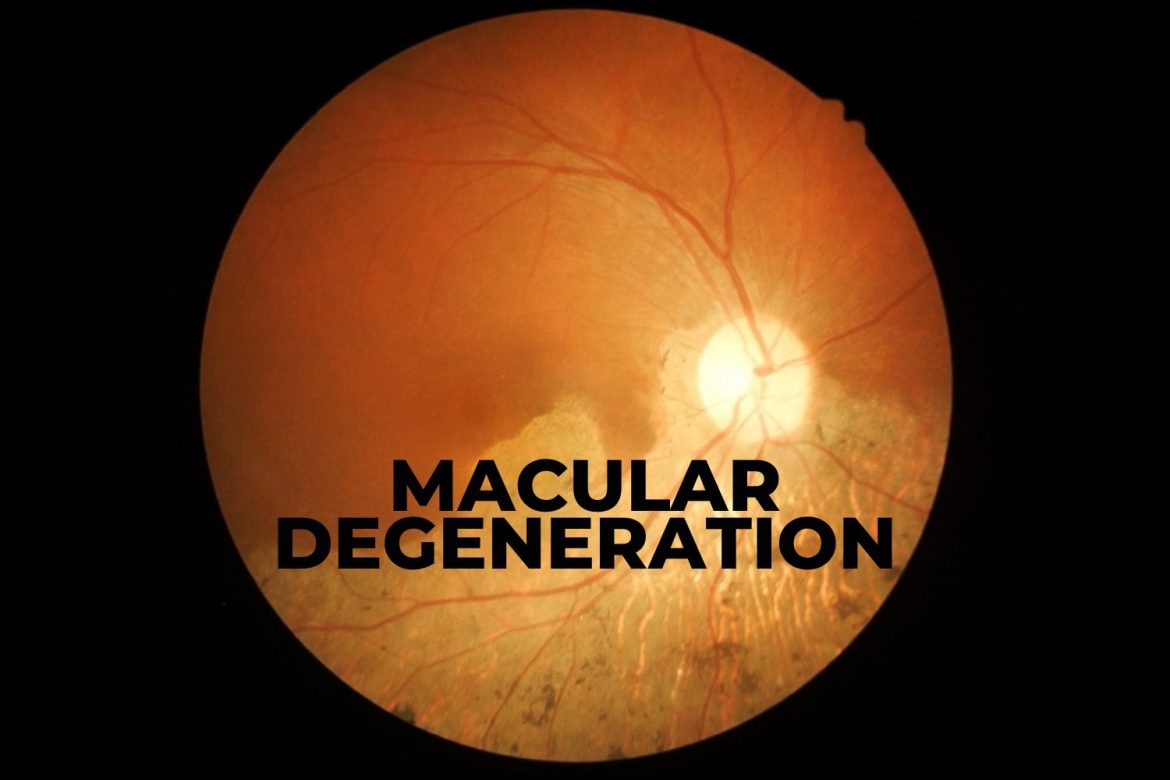
Macular degeneration is a disease that affects the part of the retina called the macula. The macula is responsible for the vision directly in your line of sight. The disease causes progressive vision loss, early signs being wavy or distorted lines in your central area of vision. Those with the disease do not go blind but may experience significant vision loss. Your side vision or peripheral vision will remain unaffected.
The disease is the leading cause of vision loss in older adults over 55 years of age. It can make it difficult to see faces, read, drive or perform other tasks.
There are two types of macular degeneration, wet and dry. The dry type can convert to the wet form with time.
Dry macular degeneration
- Most common, 90% of all cases.
- Occurs in 3 states: early, intermediate, late
- Progresses slowly over years
Wet macular degeneration
- Also called Neovascular ARMD
- Less common, 10% of cases
- Considered late-stage ARMD
- Growth of abnormal blood that leaks blood/ fluid underneath the retina
- Causes significant vision loss
- May progress slowly or rapidly
Who is at risk for macular degeneration?
Everyone’s risk increases with age, but those with a family history, are Caucasian, have a high BMI, and/or smoke, have an increased risk although to what extent is unknown.
In addition, there are some indications that lower socioeconomic status and less education are associated with more advanced ARMD.
How is macular degeneration diagnosed?

Macular degeneration can be diagnosed by your doctor by looking at the back of your eye with a dilated fundus exam. Drusen is the first sign of macular degeneration. Drusen can be thought of as waste product that remains in the retina. It appears as yellow deposits that lie underneath the retina. Drusen can appear in various sizes and shapes. Small drusen are not treated, but indicate more of a risk of conversion to wet macular degeneration and should be monitored.
Wet macular degeneration may also be diagnosed by a dilated fundus exam but may need confirmation using more advanced technologies and imaging. Your doctor may perform two types of routine tests, fluorescein angiography and optical coherence tomography (OCT).
Fluorescein angiography
Fluorescein Angiography uses a dye and camera to look at blood flow in the retina.
Optical coherence tomography (OCT)
An OCT uses light rays to detect which layer of the retina is affected by the disease.
How do you prevent macular degeneration?
Though your genetics play a role in macular degeneration, there are some modifications you can make in your lifestyle and environment that may reduce your risk of the disease.
Don’t smoke
Smoking is a major risk factor for developing a more severe type of ARMD, wet ARMD. Current smokers of 20 or more cigarettes per day had a 2X-fold increase in risk compared with those who had never smoked.
Maintain a healthy blood pressure
There is a connection between cardiovascular disease (high blood pressure, cholesterol) and ARMD. Some studies demonstrate that patients with wet ARMD are at a higher risk of stroke confirming there are common factors between the two diseases.
Healthy diet

A healthy diet filled with the carotenoids found in dark green, leafy vegetables has the potential to decrease your risk. A carotenoid called Lutein reduces inflammation in the eye; spinach and bell peppers are always recommended to patients with early signs of ARMD. Other foods high in Lutein include kale, romaine lettuce, corn, parsley, pistachios, and eggs,
Regular exercise
Although a weak association, excess body weight increases the risk of AMD. Maintaining a healthy BMI and avoiding weight gain may protect against ARMD. In fact, exercise may reduce your risk of developing ARMD by up to 70%.
How is macular degeneration treated?
The treatment depends on the type of macular degeneration you have, the stage of the disease, and if it is progressing. Treatment is designed to slow progression and prevent vision loss.
Dry macular degeneration should be monitored frequently by a doctor and is treated with ARMD-specific nutraceuticals. Your doctor will give you an Amsler grid, comprised of a series of squares, for you to monitor vision changes at home. If you notice any distortions or changes in wavy lines, you should let your doctor know ASAP.
A new drug called Pegcetacoplan is currently in clinical trials for the treatment of late-stage dry ARMD called geographic atrophy. The drug was able to reduce the size of the lesions and is expected to be available for patients in 2022. This is quite promising!
Wet macular degeneration can be treated using anti-angiogenic drugs or laser therapy.
Anti-angiogenic drugs
Anti-angiogenic drugs are injected into your eye to stop new blood vessels from forming and abnormal vessels from leaking.
Laser therapy
Lasers can be used to destroy abnormal, leaky blood vessels.
Can your vision be improved when you have macular degeneration?
Unfortunately, your vision with macular degeneration can rarely be improved with glasses or contacts. Devices can be used to maximize your remaining vision. Specialty magnifiers, large print devices, phone apps, and a device called a CCTV can move images to the healthy parts of your retina allowing you to pursue hobbies you may have given up, such as reading.
Though we remain without a cure for macular degeneration, there is promising research on the horizon. More research has been dedicated to the cause of the disease and possible treatments. Currently, a low vision specialist can help maximize your vision by recommending devices and technology to maintain your independence.